Can Allergies Cause Sleep Apnea?
Learn why allergies might be an indicator for a more serious issue like sleep apnea, how these conditions overlap, and how to treat them together.

Sometimes my patients think they’re just having trouble breathing at night because of seasonal allergies, without realizing they may actually be suffering from sleep apnea.
There are a few misconceptions regarding how seasonal allergies (aka “allergic rhinitis”) and sleep apnea relate to each other.
Can allergies cause obstructive sleep apnea (OSA)? Probably not.1, 2, 3
But could they make sleep apnea symptoms worse? Yes, that’s possible.4
About 54 million Americans suffer sleep apnea, but only a few million of them have been formally diagnosed. If you have mild sleep apnea symptoms that you’ve been ignoring, allergy season might be making your condition worse.
While that doesn’t seem like a good thing, it provides additional opportunities to navigate your health. So let’s dive in so we can understand how these two conditions relate to each other.
Learn More: What is sleep apnea?
How Allergies Make Sleep Apnea Worse
Generally, we’re supposed to breathe through our noses because this allows air to get warmed up and humidified on the way to our lungs for better oxygen extraction.
Allergies tend to make sleep apnea worse because they cause inflammation and congestion in the upper airway, further reducing airflow.5
Though a few studies have suggested that allergic rhinitis could cause sleep apnea through this mechanism,6, 7 it’s more likely that seasonal allergies just make existing sleep apnea worse.4
Anything that makes your airway more narrow can make “apneic” episodes longer or more frequent. So if you’re suffering a lot of congestion and sneezing during allergy season, the severity of your sleep apnea is likely going to worsen as well.
Related: What happens to your body during a sleep apnea episode?
Aside from its effects on your airway, you’re also more likely to suffer from interruptions in your sleep due to snoring, drainage, and other discomforting symptoms—especially considering that allergies are usually worse at night.
This is why we routinely recommend tackling allergies when we treat sleep apnea.
How Allergy Treatment Impacts Sleep Apnea
If you struggle with seasonal allergies, you've probably spent a fair amount of time in the allergy aisle at your local drugstore. You may have tested a fair number of medications and may even have a favorite brand. But if you have diagnosed sleep apnea—or even suspect sleep apnea—it's important to be aware of how common Over-The-Counter allergy medications affect the condition.
Medications to avoid if you suspect sleep apnea
Antihistamines reduce your body’s immune response to whatever you’re allergic to, which is why they’re popular with allergy patients. That said, if you have sleep apnea, they are not without their risks.
In particular, first-generation antihistamines have a negative effect on sleep cycles. And all antihistamines have been associated with weight gain, which is known to worsen sleep apnea.8 Examples include:
Benadryl
Claritin
Zyrtec
Xyzal
This doesn’t mean you can’t use these medications at all. But if you've been diagnosed with or suspect sleep apnea, they likely aren't your best choice on a regular basis.
If you find your allergies persist more than a few days at a time or don’t respond well to other medications, it’s probably time to talk to your doctor about prescription treatment options.
Alternative Medications that don't negatively impact sleep apnea
In the meantime, if you're struggling with allergy season, these medication options are relatively fine or neutral with regard to sleep apnea:
Decongestants like Sudafed, Tylenol Sinus, or Advil Cold and Sinus
Intranasal steroids like Flonase or Nasacort
Is it possible that I just have allergies and not sleep apnea?
If it’s allergy season and your spouse is complaining about your snoring, you may be tempted to think it’s “just allergies.” Snoring by itself can be explained by seasonal allergies—especially if it’s temporary, and you’re not usually a snorer.
But if your year-round snoring has gotten worse, sleep apnea could be the cause. Especially if it’s combined with symptoms like these:
Audible gasping or choking in your sleep
Daytime tiredness
Dry mouth
Depression/anxiety
Low libido or erectile dysfunction
Why You Should Be Concerned about Sleep Apnea
Unfortunately, if you have persistent snoring and some of the other symptoms mentioned above, it means there’s a good chance you have sleep apnea, which has long-term implications for your health. Patients who don’t treat their sleep apnea are likely to suffer from a variety of major health conditions like:
Diabetes
Heart Disease
Stroke
The good news is that treating your sleep apnea could stop, and in some cases, reverse your risk for developing these conditions.
Learn More: What are my options for treating sleep apnea?
“Just Allergies” or Something More?
It’s not possible to distinguish between allergy-related snoring and sleep apnea just by what you sound or look like while you’re sleeping. If you’ve tried treating your allergies and have seen improvements in your congestion, but still struggle with snoring and sleepiness during the day, it might be time for a deeper evaluation.
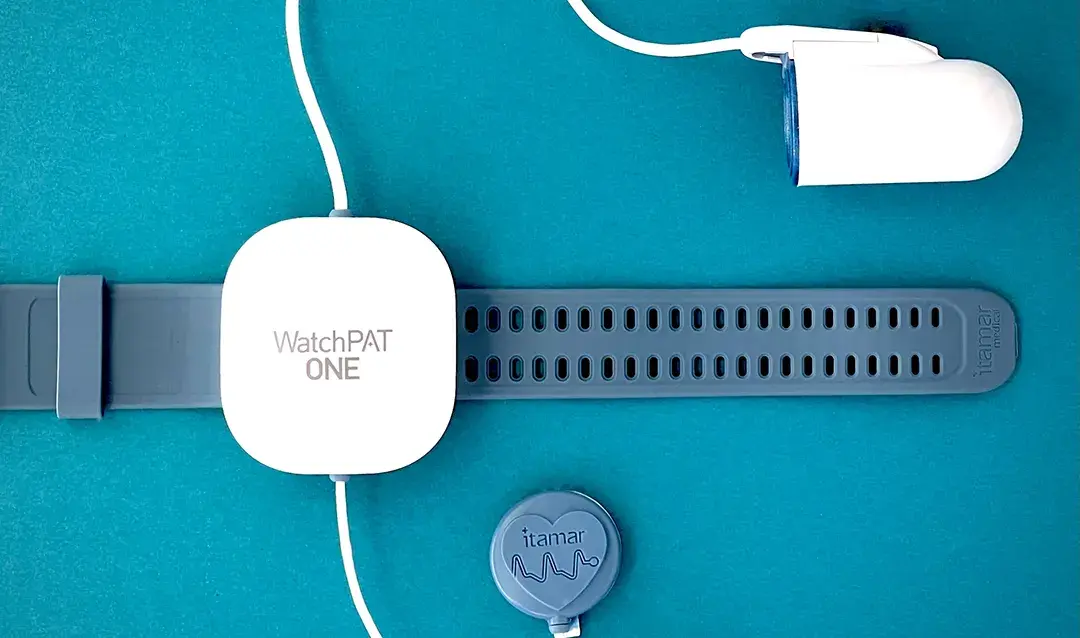
Our free, 5-minute sleep assessment is a great starting place to identify your risk level for sleep apnea. If you find that you're high risk for the condition, an at-home sleep test will be your next step to solving sleep apnea for good.
If treating your allergies and snoring has improved your sleep, just wait to see how much better you’ll feel after treating your sleep apnea.
Zheng M, Wang X, Ge S, Gu Y, Ding X, Zhang Y, Ye J, Zhang L. Allergic and Non-Allergic Rhinitis Are Common in Obstructive Sleep Apnea but Not Associated With Disease Severity. J Clin Sleep Med. 2017 Aug 15;13(8):959-966. doi: 10.5664/jcsm.6694. PMID: 28633721; PMCID: PMC5529132. Available from: https://pubmed.ncbi.nlm.nih.gov/28633721/
Cao Y, Wu S, Zhang L, Yang Y, Cao S, Li Q. Association of allergic rhinitis with obstructive sleep apnea: A meta-analysis. Medicine (Baltimore). 2018 Dec;97(51):e13783. doi: 10.1097/MD.0000000000013783. PMID: 30572534; PMCID: PMC6319794. Available from: https://pubmed.ncbi.nlm.nih.gov/30572534/
Liu J, Zhang X, Zhao Y, Wang Y. The association between allergic rhinitis and sleep: A systematic review and meta-analysis of observational studies. PLOS ONE. 2020;15(2):e0228533. doi:10.1371/journal.pone.0228533 Available from: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0228533
Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea. [Updated 2022 Dec 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459252/
Akhouri S, House SA. Allergic Rhinitis. [Updated 2023 Jul 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538186/
Nguyen-Hoang Y, Nguyen-Thi-Dieu T, Duong-Quy S. Study of the clinical and functional characteristics of asthmatic children with obstructive sleep apnea. J Asthma Allergy. 2017 Oct 12;10:285-292. doi: 10.2147/JAA.S147005. PMID: 29066920; PMCID: PMC5644536. Available from: https://pubmed.ncbi.nlm.nih.gov/29066920/
McNicholas WT, Tarlo S, Cole P, Zamel N, Rutherford R, Griffin D, Phillipson EA. Obstructive apneas during sleep in patients with seasonal allergic rhinitis. Am Rev Respir Dis. 1982 Oct;126(4):625-8. doi: 10.1164/arrd.1982.126.4.625. PMID: 7125355. Available from: https://pubmed.ncbi.nlm.nih.gov/7125355/
Jullian-Desayes I, Revol B, Chareyre E, Camus P, Villier C, Borel JC, Pepin JL, Joyeux-Faure M. Impact of concomitant medications on obstructive sleep apnoea. Br J Clin Pharmacol. 2017 Apr;83(4):688-708. doi: 10.1111/bcp.13153. Epub 2016 Nov 24. PMID: 27735059; PMCID: PMC5346880. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5346880/