Central Sleep Apnea vs Obstructive Sleep Apnea: What's the Difference?
A sleep doctor explains the differences between central and obstructive sleep apnea, their root causes, and treatment options for each.

As patients pursue treatment for sleep apnea, many can find themselves hung up on two different conditions: obstructive sleep apnea (OSA) and central sleep apnea (CSA).
OSA is far more common than CSA—enough so that physicians tend to rule out obstructive sleep apnea before considering central apnea. Still, the two conditions occur for different reasons and result in different treatment, so it’s important to understand the distinction.
What exactly is an “apnea?”
Before diving into the differences between OSA and CSA, let's start with the basics. Both conditions share a commonality: frequent apneas. An "apnea" simply refers to a pause in breathing during sleep.
Learn More: Sleep Apnea 101
From a clinical perspective, this pause is officially labeled as an "apneic episode" if your breathing pauses for at least ten seconds while you’re sleeping. If that’s happening more than five times an hour, we officially diagnose it as either CSA or OSA.
Understanding Obstructive Sleep Apnea (OSA)
As the name implies, obstructive sleep apnea episodes are caused by an obstruction—or blockage—of your airway while you sleep. This is a physical issue, in which the relaxation and narrowing of your upper airway leads to repeated apneic events.
Related: What is an apneic event?
When this happens, your body triggers a fight-or-flight response, jolting you awake. These are brief arousals, so you may not even remember waking up. But these repeated apneic events wreak havoc on your sleep cycle, resulting in a range of downstream health issues.
How Central Sleep Apnea (CSA) Differs
Rather than a physical obstruction, think of central sleep apnea (CSA) as an 'electrical' glitch. It happens when your central nervous system fails to send the signal to your muscles to trigger a breath.
In either case, your body will eventually trigger the same fight or flight response to wake you up so you start breathing again—but the apneic event is based on a different root cause.
Do Risk Factors Vary?
A number of factors can cause the ‘obstruction’ aspect of OSA, including your weight, alcohol use, genetics, the shape of your soft palate, and whether you sleep on your back, side, or stomach.
Related: Who is at risk for obstructive sleep apnea?
Risk factors for Central Sleep Apnea tend to be more intricate, involving various medical conditions, medication usage, and and the body's regulation of carbon dioxide levels, among other complexities.1
Key contributing factors for CSA include:
Heart health issues, such as heart failure or unusual heart rhythms like atrial fibrillation.
Neurological conditions, ranging from certain types of sclerosis and brainstem-affecting strokes to spinal cord injuries.
Ingestion of certain substances, including alcohol, narcotics, and various sedatives.
Surprisingly, treatment for OSA, notably CPAP therapy, can sometimes trigger central sleep apnea. This phenomenon is known as "treatment-emergent sleep apnea."
No matter the cause, though, sleep apnea treatment options are available to help restore a functioning airway and normal breathing patterns while you sleep.
Comparing Prevalence Rates
Obstructive sleep apnea is widespread, affecting up to 38% of the population2, whereas central sleep apnea is much less common, with prevalence rates estimated at only 0.9% among individuals over 40.3 Cases diagnosed as OSA may sometimes include central apnea components, termed "mixed apnea," but this occurrence is still relatively rare, affecting around 2.7% of the general population.3
Given this huge disparity in prevalence, central sleep apnea tends not to be our first consideration as providers unless there are other major medical problems to suggest it might be present.
Symptoms and Long-Term Health Outcomes
Since both CSA and OSA share the presence of apneic events, symptoms and health outcomes from the two conditions tend to overlap. Symptoms of sleep apnea in any form tend to include disrupted sleep patterns, daytime sleepiness, fatigue, and morning headaches. Long-term health risks associated with both conditions stem from oxygen level drops, frequent arousals, and interrupted sleep cycles, leading to similar health outcomes.
How are obstructive and central sleep apnea diagnosed?
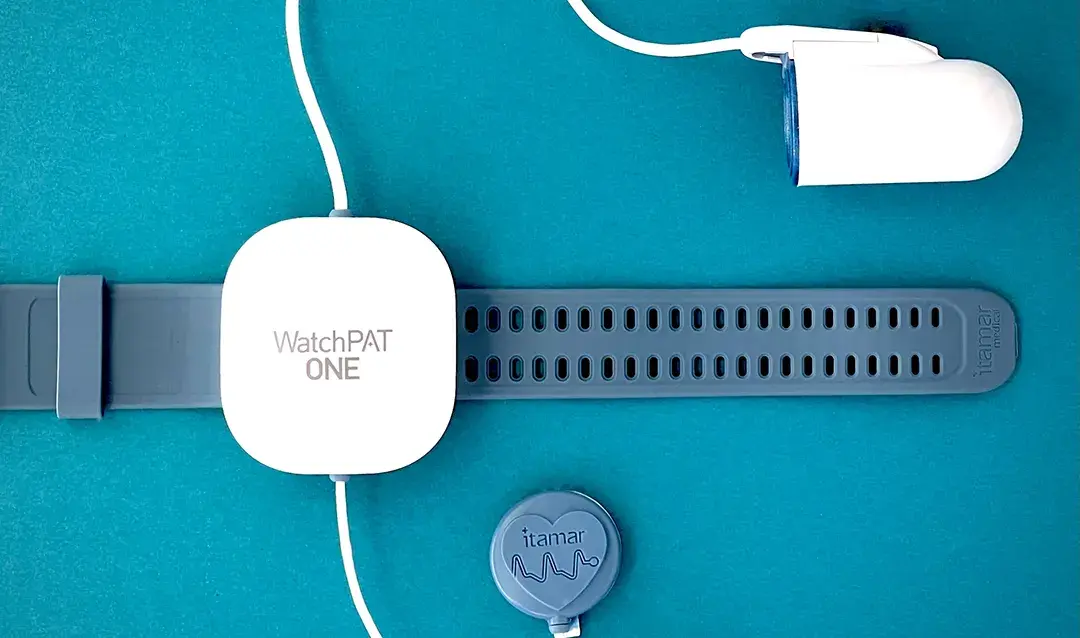
Sleep apnea is diagnosed using a sleep study, either at home or in a lab. The sleep study detects apnea by measuring the number of pauses in breathing that last for ten seconds or longer, along with drops in blood oxygen level.
Related: Are home sleep apnea tests as good as lab tests?
If that pause is associated with signs of respiratory effort (like chest movement), we know it’s obstructive sleep apnea. If there’s no detectable breathing effort, that’s our clue that central apnea may be at play. Remember, central sleep apnea means your breathing muscles aren’t ever getting the signal to trigger a breath—so when that happens, we wouldn’t detect breathing effort.
The central apnea event may be validated with other measurements, but this is the basic idea of how we identify them.
Can a home study detect central sleep apnea?
Some, though not all, home sleep tests can detect central sleep apnea. However, if your physician detects central apnea, they may recommend an in-lab overnight study. Again, obstructive sleep apnea is the far more common condition and can be diagnosed with high accuracy using an at-home test. So in most cases, doctors tend to recommend at-home tests for sleep apnea diagnosis.
Navigating Treatment Options
Your options for sleep apnea treatment will depend largely on how severe your condition is and what treatment plan you can realistically stick to. That said, the type of sleep apnea you’re diagnosed with—central vs. obstructive sleep apnea—will have some impact on your treatment plan.
Learn More: Sleep Apnea Treatment Options Explained
Treatment for Obstructive Sleep Apnea
Historically, CPAP (continuous positive airway pressure) devices have been the predominant treatment for obstructive sleep apnea, as these devices are extremely effective at keeping the airway open while the patient is asleep. However, many patients find this treatment method uncomfortable and struggle to maintain treatment over time—so alternative treatment options are becoming more common.
Oral appliances, similar to retainers, are a popular and more comfortable alternative for obstructive sleep apnea treatment. These devices work by repositioning the jaw and tongue to keep the airway open while sleeping.
Treatment for Central Sleep Apnea
Since central sleep apnea is often linked to other health issues or medication side effects, our first step in treatment targets these root causes—sometimes requiring lifestyle adjustments.
Further treatment options can include positive airway pressure (PAP) therapy, supplemental oxygen, medication, or (less frequently) an implantable nerve stimulation device. Oral appliances don’t address the root cause of central sleep apnea, so they aren’t a primary treatment when exclusively CSA is indicated.
Remember, though, that many patients with CSA also have obsctructive apnea. When that’s the case, a mix of treatment options—possibly including an oral appliance—could be suggested.
As you can see, there’s a lot to consider when determining treatment for central or obstructive sleep apnea. This is why it’s important to walk alongside a board-certified sleep physician who can identify the nuances of your situation and make recommendations that have a higher chance of being effective.
Rana AM, Sankari A. Central Sleep Apnea. [Updated 2023 Jun 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK578199/
Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev. 2017 Aug;34:70-81. doi: 10.1016/j.smrv.2016.07.002. Epub 2016 Jul 18. PMID: 27568340. Available from: https://www.sciencedirect.com/science/article/abs/pii/S1087079216300648
Donovan LM, Kapur VK. Prevalence and Characteristics of Central Compared to Obstructive Sleep Apnea: Analyses from the Sleep Heart Health Study Cohort. Sleep. 2016 Jul 1;39(7):1353-9. doi: 10.5665/sleep.5962. PMID: 27166235; PMCID: PMC4909617. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909617/