What happens to your body during a sleep apnea episode?
A deep dive into the dangerous 10 seconds of suffocation you may be facing up to hundreds of times per night.

If you’ve heard of sleep apnea, you might know that it makes you stop breathing while you’re sleeping. But, if we’re being honest, that can sound hard to believe.
“What do you mean, I 'stop breathing'? I would remember something like that!”
The truth is that an “apneic event”—or one episode of a pause in breathing—usually doesn’t wake you up enough to fully remember that it happens. That doesn’t change the fact that there’s a whole cascade of events triggered by the body to get you to start breathing again.
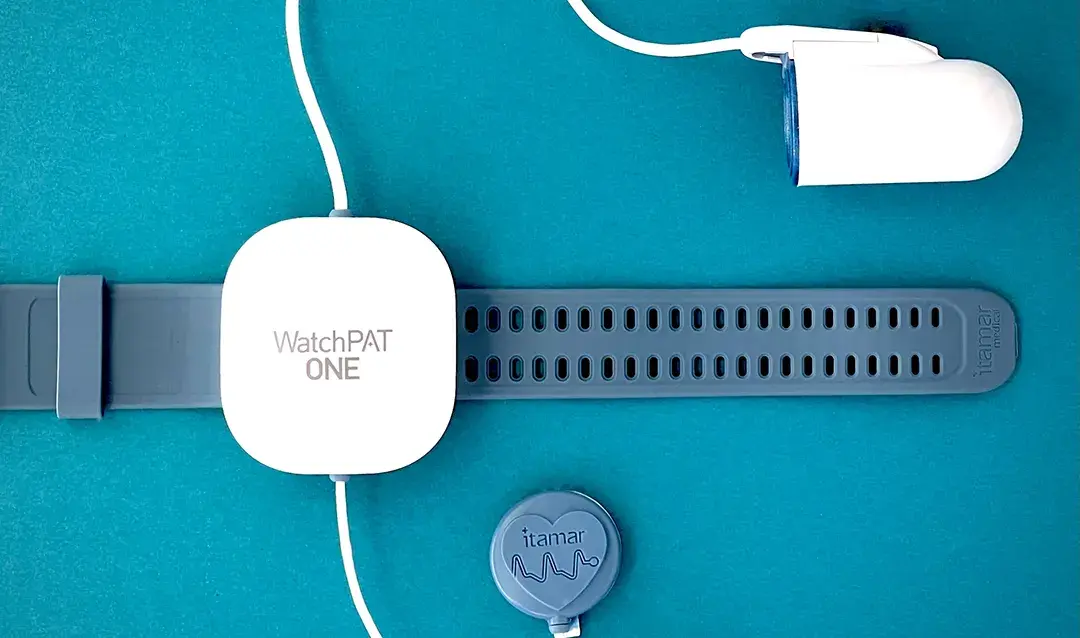
In clinical sleep apnea, this happens a lot throughout the night. To measure the exact frequency, we use an at-home sleep test to count how many times per night you stop breathing for 10 seconds or longer. Each one of those incidents is an individual apneic event. That same test also measures hypopneic events, or incidents where you don't breathe deeply enough to supply adequate oxygen to your organs. Together, the measurement of those breathing dips determine your Apnea Hypopnea Index (AHI)—calculated as the number of apnea or hypopnea events per hour. Your AHI tells us the overall severity of your sleep apnea:
Mild sleep apnea consists of an AHI of 5-14 events per hour
Moderate sleep apnea consists of an AHI of 15-29 events per hour
Severe sleep apnea consists of an AHI of 30 or more events per hour
This means, even if you just have a mild to moderate case of sleep apnea, you stop breathing 40 - 232 times a night! When you stop breathing even just once, the body responds in a number of ways, all with the end goal of getting you to breathe again. So let’s see what happens before, during, and after one of these episodes.
Please note: this cascade of events describes a typical obstructive sleep apnea episode rather than an episode of central sleep apnea. While these look different, obstructive sleep apnea will be described since it is the most common form.
Step #1: You fall asleep.
It probably seems obvious that sleep apnea happens when you’re asleep. That said, it is an important fact to consider since there are similar illnesses like “obesity hypoventilation syndrome,” which are present when you’re asleep and when you’re awake.
Step #2: Your airway relaxes.
Sleep apnea causes you to stop breathing (ie., an “apnea”) or not breathe deeply enough (i.e., a “hypopnea”). This can happen for a lot of reasons, but the most common is that the muscles around your upper airway relax and collapse, leading to a pause in breathing. This is called an “apneic event.”
“But why is my airway relaxing?”
In normal sleep stages, your whole body is semi-paralyzed so that you don’t act out your dreams physically. But when you have sleep apnea, the paralysis can also affect your airway, which you may be more prone to if you have one of several issues that can make your airway smaller or more likely to collapse - things like obesity (which causes an increase in fatty tissue around your airway), several anatomical abnormalities, and alcohol consumption, among others.1
Step #3: Your oxygen drops and carbon dioxide rises.
At this point, you’ve stopped breathing for at least 10 seconds (the threshold length for an “apneic event”), and you’re probably not surprised that what happens at this point is that your blood oxygen levels start dropping. However, what you may not know is that, during normal breathing, you blow carbon dioxide out of your lungs with each breath. As a result, when you stop breathing due to sleep apnea, your carbon dioxide levels are starting to rise as well.
Step #4: Your brain responds with “fight or flight” signals.
High carbon dioxide and low oxygen are mission-critical signals for the brain - after all, you need a constant supply of oxygen for every single function your body performs. Because this is now becoming a life-threatening situation, your body triggers a “fight or flight” response.
In medicine, we call this a “sympathetic” response, and it involves the release of adrenaline, cortisol, and other hormones to trigger a cascade of events affecting many major organs.2
Step #5: You experience a microarousal.
During a microarousal, you wake up partially from deep sleep, but usually not enough to fully regain consciousness.3 Microarousals are much more common than full awakenings, which is why most people don’t remember this occurring throughout the night.
Step #6: You start breathing deeper and faster.
This is probably a familiar feeling—if you’ve ever been nervous, scared, or anxious, this triggers the exact same “sympathetic response” we’ve been talking about. And if you’ve ever been in a situation like that, you probably remember breathing faster.
In the context of sleep apnea, your body is using this response in an attempt to overcome the collapsed airway.
Step #7: Your body increases muscular tension.
Remember, an “apneic event” happens when the muscles around your airway relax and collapse. As part of the sympathetic response, your body quickly regulates hormones like norepinephrine and acetylcholine to increase overall muscle tone, which helps your airway to open up again.4
Step #8: Your breathing returns to normal - for a while.
At this point, the body has corrected the pause in breathing, and you slowly go back into a deeper sleep. No harm, no foul, right? Not exactly. Remember, all this happened when you stopped breathing just once, but these pauses in breathing are happening potentially hundreds of times a night.
The reason all this is a problem is because the frequent interruption in normal sleep cycles and the repeated activation of a system that’s designed to help you run away from dangerous animals takes a toll on your body over time, and usually in ways that are much bigger than just feeling tired.
Luckily, there are options for treating sleep apnea. One of them is a custom-fitted oral device similar to a nightguard which helps keep your airway open while you sleep. With the right treatment, you can easily treat your sleep apnea and avoid this dangerous cascade of events entirely.
Osman AM, Carter SG, Carberry JC, Eckert DJ. Obstructive sleep apnea: current perspectives. Nat Sci Sleep. 2018 Jan 23;10:21-34. doi: 10.2147/NSS.S124657. PMID: 29416383; PMCID: PMC5789079.
Narkiewicz K, Somers VK. The sympathetic nervous system and obstructive sleep apnea: implications for hypertension. J Hypertens. 1997 Dec;15(12 Pt 2):1613-9. doi: 10.1097/00004872-199715120-00062. PMID: 9488212.
Ren R, Zhang Y, Yang L, Somers VK, Covassin N, Tang X. Association Between Arousals During Sleep and Hypertension Among Patients With Obstructive Sleep Apnea. J Am Heart Assoc. 2022 Jan 4;11(1):e022141. doi: 10.1161/JAHA.121.022141. Epub 2021 Dec 31. PMID: 34970921; PMCID: PMC9075207.
Goya TT, Silva RF, Guerra RS, Lima MF, Barbosa ER, Cunha PJ, Lobo DM, Buchpiguel CA, Busatto-Filho G, Negrão CE, Lorenzi-Filho G, Ueno-Pardi LM. Increased Muscle Sympathetic Nerve Activity and Impaired Executive Performance Capacity in Obstructive Sleep Apnea. Sleep. 2016 Jan 1;39(1):25-33. doi: 10.5665/sleep.5310. PMID: 26237773; PMCID: PMC4678332.